In this section
In This Section
What is radiotherapy?


Radiotherapy is the use of ionising radiation, usually high energy x-rays to treat disease. Radiotherapy is usually used to treat malignant disease (cancer). It is sometimes used to treat benign tumours and some benign diseases.
Radiotherapy treatment is often split into a number of treatments or fractions. These are usually given over a number of days. This allows larger doses of radiation to be given and reduces the amount of normal tissue being treated which can reduce the side effects experienced by patients. Radical treatments are given in more treatment fractions than palliative.
For more general information about radiotherapy visit the Macmillan Cancer Support website. Also see the Cancer Research UK information and video about why radiotherapy is so important.
Radiotherapy staff
Therapeutic radiographer
These are specialist health care professionals qualified in the localisation and treatment of cancer using ionising radiation (as distinct from diagnostic radiographers who image patients for diagnosis). Therapeutic radiographers' levels of practice range from practitioner through to advanced, and to highly specialised consultant roles.
Clinical oncologist
Medical consultants qualified in the treatment of cancer using radiotherapy, chemotherapy and hormone therapy. They usually specialise in the treatment of certain cancers.
Physicist / clinical scientist
Medical physicists who work in radiotherapy supervise the dose of radiation delivered to treat cancer patients. They are responsible for commissioning, calibration, safe operation and maintenance of radiotherapy equipment. They are involved in planning complex treatment for individual patients using a range of complex equipment which includes linear accelerators. They also have a role in ensuring a safe environment for patients and staff from potential hazards including radiation.
Clinical technologists including dosimetrists
Clinical technologists (also known as medical technologists) are responsible for maintaining, monitoring and sometimes operating the equipment and instruments used to treat radiotherapy patients. They are trained in clinical physics. Roles vary, and include being responsible for the production of individual patient treatment plans, quality assurance testing of radiotherapy equipment, equipment maintenance and engineering support.
Clinical engineer
Clinical engineers design and test the tools and equipment that the radiotherapy team use to carry out radiotherapy planning and treatment procedures. They work closely with clinical scientists, physicists and technologists.
Support staff
There is a variety of staff who support the radiotherapy service. These include clerks, secretarial and administrative staff, clinic helpers and support workers. They ensure the smooth running of the service.
How important is radiotherapy in the treatment of cancer?
Surgery is the most effective way of curing cancer with 49% of all patients cured of cancer being cured by surgery. Some key facts about radiotherapy include:
- After surgery, it is the next most important method of curing cancer.
- 40% of all patients cured of cancer are cured by radiotherapy.
- 50% of all cancer patients will benefit from receiving radiotherapy as part of their cancer management.
- It can offer patients the choice of organ preservation and avoid the need for disfiguring or damaging surgery: For example, instead of mastectomy for breast cancer, conservation radiotherapy can be given. Radiotherapy can also be used for the treatment of certain cancers of internal organs and allow patients to avoid major surgery and retain function, with little or no loss of chance of cure. Examples of this would include cancers of the larynx, prostate and bladder.
- Its use is continuing to expand. This is due to better patient pathways, the role of multi-disciplinary team meetings and more integrated treatments.
- In the last decade technology has advanced and radiotherapy has become more sophisticated. This has enabled the delivery of more targeted treatments.
- Timely access to radiotherapy leads to improvements in cancer outcome and survival rates.
Can radiotherapy be given with other treatments such as chemotherapy?
Yes, radiotherapy is often given with chemotherapy (radiochemotherapy or chemoradiotherapy). This can enhance the effect of the radiotherapy. This is now standard treatment for some cancers, such as those of the oesophagus or uterine cervix. It is likely to be used for more cancers as the results of clinical trials prove that the outcomes for patients having these treatments is improved.
The role of the therapeutic radiographer in the delivery of these modalities when combined is important so as to gain their maximum effect.
What sorts of radiotherapy are there?
Radiotherapy can be delivered by two main methods:
External radiotherapy
This is delivered by using radiation sources from outside of the body. The types of treatments most frequently used are:
- High energy x-rays. Delivered using linear accelerators. The most modern machines have facilities to treat the latest techniques such as Intensity Modulated Radiotherapy (IMRT), Image Guided Radiotherapy (IGRT) and 4D adaptive radiotherapy.
- Superficial beam radiotherapy. The use of low energy x-rays or electrons to treat skin cancers.
- Proton beam therapy. This is not yet available in the UK. For patients England the DofH has a patient referral pathway to centres in Europe and USA. There are treatment centres being planned in England, these will be available in 2017. More information about the referral process for proton treatment is available on this website.
There are other more specialised radiotherapy treatments such as stereotactic radiotherapy, total body irradiation and intraoperative radiotherapy.
Once your health care team has decided which treatment is most suitable for you they will explain the planning and treatment procedures and any likely side effects you may happen to you.
For more information about radiotherapy see the information in the Macmillan Cancer Support website.
Internal radiotherapy
This is the use of a radioactive material placed within the body. There are two ways to do this:
- Brachytherapy. This is the use of specially designed equipment to allow a radioactive sources to site inside the patient for a specific time and place to deliver the required dose of radiation. This is often used for the treatment of patients with cancer of the cervix, uterus, oesophagus and prostate.
- Radioisotope treatment. The use of a radioactive liquid which is either given as a drink or an injection. This may be used to treat cancer of the thyroid and secondary cancer which has spread to the bones.
For more information about these techniques see the information on the Macmillan Cancer Support website about internal radiotherapy.
What is the radiotherapy process? What will happen to me?
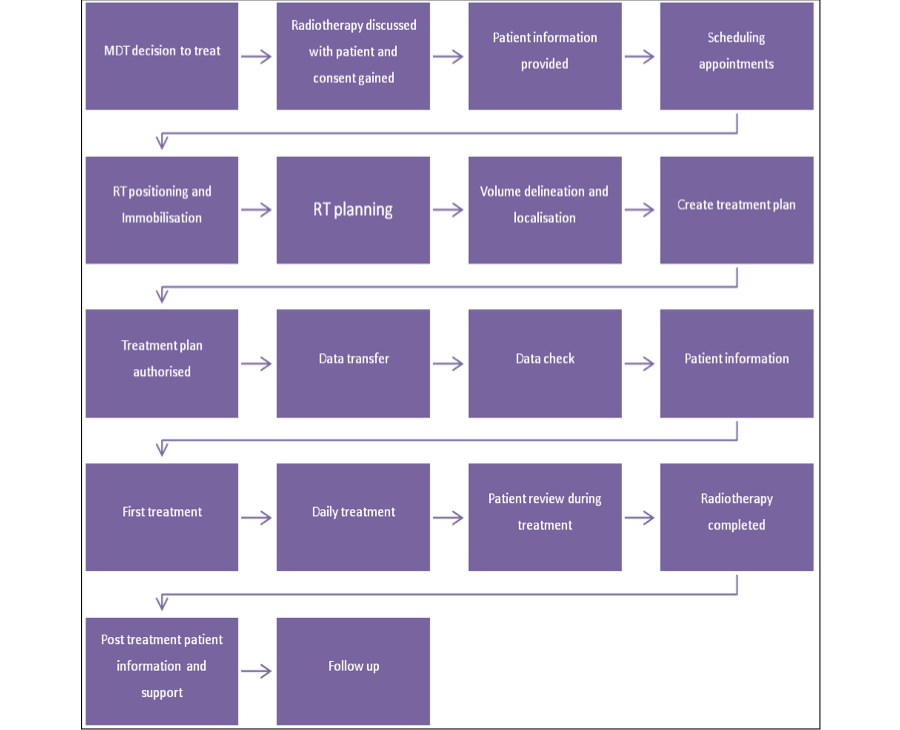
The delivery of radiotherapy is a complex process and careful preparation is necessary before treatment can begin. The planning of radiotherapy is a very important part of radiotherapy and it may take a few visits.
There are many steps involved in providing radiotherapy treatment to patients and the complexity of this journey with each of the stages is illustrated in the simple diagram below.
Many of the national cancer charities provide detailed information about radiotherapy. You may find it useful to visit their websites. Three examples are suggested below:
- Macmillan Cancer Support online DVD explaining radiotherapy.
- Cancer Help UK provides reliable and easy to understand information from Cancer Research UK. There are several video clips on this website explaining various aspects of radiotherapy; radiotherapy planning, having a mask made, having radiotherapy, having radiotherapy for brain or head and neck cancer.
- A guide for children on You Tube called “One of a kind! A kind of radiotherapy”. This uses cartoon characters to explain radiotherapy to children.
Please ask at your cancer centre about the different stages you will have to undertake to have your treatment.
How do I know how my local radiotherapy service compares with others?
ENGLAND
In England the Department of Health document: Improving Outcomes: A Strategy for Cancer sets out an ambitious vision for the delivery of the world class cancer services. The most recent report: Radiotherapy Services in England 2012 is available from the download section below.
From 1 April 2013 the strategic planning of specialised services for the NHS Commissioning Board (NHS CB) will be informed by bringing specialised expertise and advice together with the views of patients and their carers in the form of service-specific Clinical Reference Groups (CRGs). The Radiotherapy Clinical Reference Group (CRG) is within the Cancer & Blood programme. This is being established and will be responsible for setting the national standards of care for radiotherapy, services will therefore be commissioned against these standards. Chairs : Dr Nick Slevin (Clinical Oncologist, Christie).
SCOTLAND
WALES
National audit reports are available fromThe National Specialist Advisory Group for Cancer.
National Standards for Cancer Services are also available.
NORTHERN IRELAND
The Service Framework for Cancer Prevention, Treatment and Care sets out recommendations and actions for the strengthening of cancer services in Northern Ireland and also sets standards for the delivery of cancer services is available in the download section below.
